 Contact Us
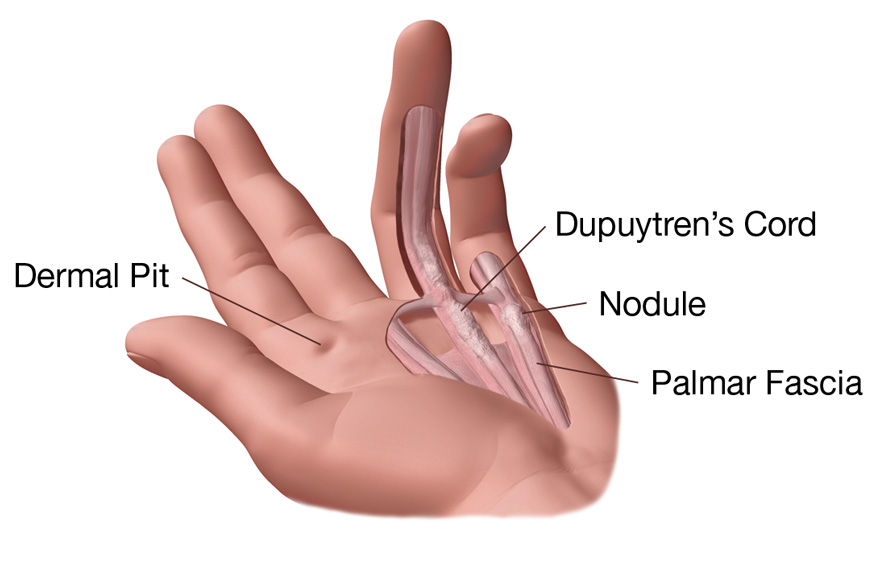
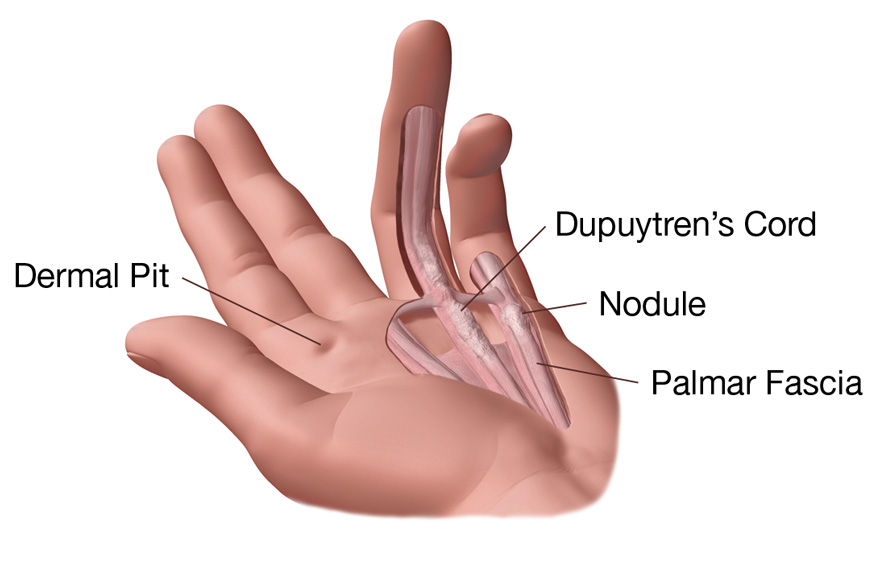
Contact UsDupuytren's disease was first described in 1831 by famous French surgeon Baron Guillaume Dupuytren. Dupuytren's disease is a fibrotic tissue disorder or wound healing disorder that affects the hands. It is a non-cancerous thickening of the fascia that is characterized by the presence of excess collagen or fibrotic tissue that forms firm lumps in the palm or fingers. Indentations in the palm called dermal pits are also common. The lumps or dermal pits can be present for long periods of time before a cord may develop causing the fingers to contract. It is common to have the condition in both hands.
Dupuytren's disease is most common in Caucasian populations having a global prevalence of 3-6% with the highest prevalence being in Scandinavia*. Countries that have seen a high level of immigration from Northern Europeans see a notably higher rate of occurance. In Austraila for example, it is estimated that 30% of people over the age of 60 are affected*. There is a strong genetic component to Dupuytren's disease. One study examined 832 relatives of 50 people with Dupuytren's disease and found that 68% of the relatives were affected by the condition*. The prevalence of Dupuytren's disease is significantly higher and develops earlier in men than women. The peak incidence is around 60-70 years in women and 50 years in men*. The age at which the condition begins often indicates the ultimate severity of the condition. Onset of the condition before the age of 30 is likely to lead to early and sever contracture of the fingers and a higher rate of recurrence after surgery*. In addition to being associated with Peyronie's disease and Plantar fibromatosis, Dupuytren's contracture is also associated with knuckle pads.
In Dupuytren’s disease, the tissue between the skin and the tendons known as the fascia becomes thickened due to a proliferation of collagen. As the collagen increases, nodules or cords are formed and the elasticity of the fascia is reduced, ultimately leading to the contracture of the fingers in some patients. In some cases the skin is also involved, but the tendons are not affected by the condition. Dupuytren's disease typically occurs slowly; however, progression may temporarily stop or rapidly progress. There are three common symptoms that people with Dupuytren's disease may experience:
As with most conditions, people may not experience all of these symptoms. For example, many people will experience nodules but will not develop any contracture of the fingers. The severity of the symptoms can also vary widely from person to person.


An exact cause of Dupuytren's disease is unknown; however, there are some potential causes that most doctors agree may play a role in the condition.
Diabetes is thought to play a large role in Dupuytren's disease. Studies have found a 3 to 33 percent prevalence of Dupuytren's in patients with diabetes; however, these patients tend to have a mild form of Dupuytren's with slow progression*. People with type 1 diabetes mellitus are at greatest risk, followed by people taking metformin and sulfonylureas*.
Trauma to the hand is thought by many doctors to cause Dupuytren's disease. The trauma may be from a blow to the hand or from certain manual jobs that expose the hands to vibration.
Many people may be genetically predisposed to fibrotic tissue disorders such as Dupuytren's disease. People of northern European descent appear to have a much higher incidence of the condition and often have a parent or a close relative with the condition. The condition is also associated with Peyronie's disease and plantar fibromatosis. About 5% of patients with Dupuytren's disease also have plantar fibromatosis, and 3% of patients with Dupuytren's disease will have Peyronie's disease.
Medications often used for treating high blood pressure that belong to the drug class known as beta adrenergic blocking agents (beta-blockers) have been reported to cause fibrotic tissue disorders. Anti-seizure medications such as phenytoin and certain supplements such as glucosamine/chondroitin and large doses of supplemental vitamin C may also promote the production of excess collagen.
A higher rate of Dupuytren's disease has been found among patients with conditions such as alcoholic liver disease, smoking, and epilepsy. While these conditions may not be a direct cause of the condition, it may indicate the impact these conditions or medications used to treat them have on wound healing.
Many different treatments for Dupuytren's disease have been used and can be divided into two major categories, invasive and non-invasive.
Most doctors agree that a non-invasive approach to treating Dupuytren's disease should be considered first given the high rate of recurrence from surgery. Invasive treatments and surgery are usually reserved for the most severe cases.